SIDE EFFECTS OF RADIATION
Apr 19, 2022
National Cancer Institute’s Common Terminology Criteria for Adverse Events V3.0 is used to describe and report acute and late toxicity attributed to radiation. This manual is used by the doctors, however it is important for all cancer patients to know about the side effects of radiation. Radiation therapy is one of the most advanced and cutting edge technology that is used for cancer treatment and management. Through this innovative technology doctors can treat a specific area without affect the nearby organs. Numerous patients have benefitted from the radiation treatment, however there are some side effects that the patients may experience. Please note that these side effects may differ from person to person.
Types of Side Effects:
SKIN: Skin reactions are commonly encountered during radiotherapy. Management of acute skin reactions should be graded according to their severity. Pruritus associated with Grade 1 and 2 skin reactions may respond to topical corticosteroids-triamcinolone ointment 0.1% BD. For moist desquamation, general principles of promoting moisture and minimizing bacterial colonization are helpful as-Open Wet Dressing, Hydrocolloid dressing, Hydrofera blue.
HEAD AND NECK:
- Mucositis – Inflammation of the mucous membranes is usually noticeable within 2-3 weeks of radiation therapy. Management of pain is essential and must be frequently reassessed during therapy. Duke’s solution and Miracle Mouthwash are helpful in oral discomfort. Benzydamine is a topical NSAID with analgesic, anti-inflammatory, anesthetic and antimicrobial properties. Smoking cessation is critical.
- Xerostomia – Major salivary glands are very sensitive to radiation damage in a dose dependent fashion. The best preventive strategy consist of excluding the parotid glands from the Radiation port when feasible. If IMRT is being used, keep the median dose of at least one parotid gland below 26 Gy. Use of Amifostine, Pilocarpine, artificial saliva, papaya extract and guaifenesin is beneficial.
- Hypothyroidism – The incidence of hypothyroidism in Head and Neck Cancers patients treated with radiation is high (50%) and increases with dose. Patients with pre-existing borderline in suffiency might be more prone to develop overt hypothyroidism after radiation.
- Trismus – Patients receiving Head and Neck Cancer radiation are at risk for developing limitation of jaw opening. Regular jaw exercises during and after radiation therapy can reduce the incidence and severity of trismus.
- Smoking – Most Head and Neck Cancers are related to tobacco use. Increase in risk of new primaries and higher treatment failure /recurrence rates in patients who continue to smoke.
- Nutrition – Certain cytokines including TNF-alpha,IL-1beta,IL-6 are postulated to elevate the so-called Resting Energy Expenditure (REE) in cancer patients. In patients with Head and Neck Cancers, treatment related side effects including mucositis, xerostomia, and trismus can further worsen their nutritional status by decreasing the caloric intake. Prophylactic advance placement of a percutaneous endoscopic gastrostomy (PEG) tube should be considered in poor health patients. Patients need approximately 2000 calories per day for an average 70 kg adult.
THORAX:
- Lung- The lung parenchyma is highly sensitive to radiation damage as by its relatively low TD 5/5 of about 17-18 Gy. During the treatment planning phase, one should try to keep V20(percentage of lung receiving at least 20 Gy), MLD(mean lung dose to total lung),NTCP(normal tissue complication probability) as law as possible. Arguably, keeping V20≤30%, MLD<20 Gy and NTCP<10% is a reasonable general strategy.
- Esophagus- Esophagitis are seen by 3rd week of radiation therapy. Primary therapy consists of antisecretory agents, analgesics, and local anesthetics.
- Heart-Radiation damage can injure different structures of the heart through the process of fibrosis, which is dose as well as volume dependent.
ABDOMEN AND PELVIS:
- Stomach – Presenting symptoms and their management are similar for acute gastritis and esophagitis and consist of antisecretory therapy. Antiemetics may be used if nausea/vomiting is present.
- Small/large bowel – Abdominopelvic radiation often produce diarrhea. If a patient develop diarrhea during therapy and there is suspicion of a possible bowel infection, this latter condition must be investigated and treated before any antidiarrheals are prescribed.
- Rectum/anus – Inflammation of rectum and anus is common during radiation. Treatment of acute proctitis and perianal reaction during radiation therapy includes use of sitz baths, steroid enema, and cream.
- Bladder – Acute , non-infectious cystitis/urethritis during radiation therapy is common & presents with dysuria, frequency and urgency.
- Prostate – Patients with urinary obstructive symptoms often experience worsening of their condition during radiation therapy. Various alpha adrenergic blockers are useful in improving urinary obstructive symptoms and represent the most frequently used pharmacological intervention.
- Penis – The risk of impotence is high in patients with prostate cancer who undergo radiation therapy. Presence of baseline erectile dysfunction, diabetes, advanced age, preceding prostatectomy, as well as use of hormonal therapy may further increase their risk.
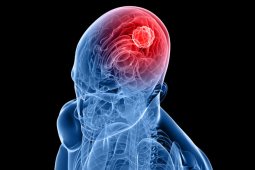
- Central Nervous System – Radiation therapy for primary or metastatic cancer involving the CNS requires use of steroids for prevention and treatment of edema.









